How to fight the coronavirus, SARS-CoV-2 and its disease, COVID-19
Michael Lin, PhD-MD
Associate Professor of Neurobiology, of Bioengineering and, by courtesy, of Chemical and Systems Biology
Stanford University
Lin Lab Briefing 2020-03-13
Revised 2020-03-20
Regularly updated here by Michael Lin
Warning: Contains facts
Bonus: Hand sanitizer recipe
This is not a pretty powerpoint
- This is an informational document.
- This is not a TED talk. It is not meant to entertain or dazzle or push an idea with beautiful graphics.
- So there will be a lot of text, because there is a lot of info that needs to be explained. Graphics will be used as data primarily. You will have to do some reading.
Some context for the numbers you will see
Total population
- 330M USA
- 40M California (CA)
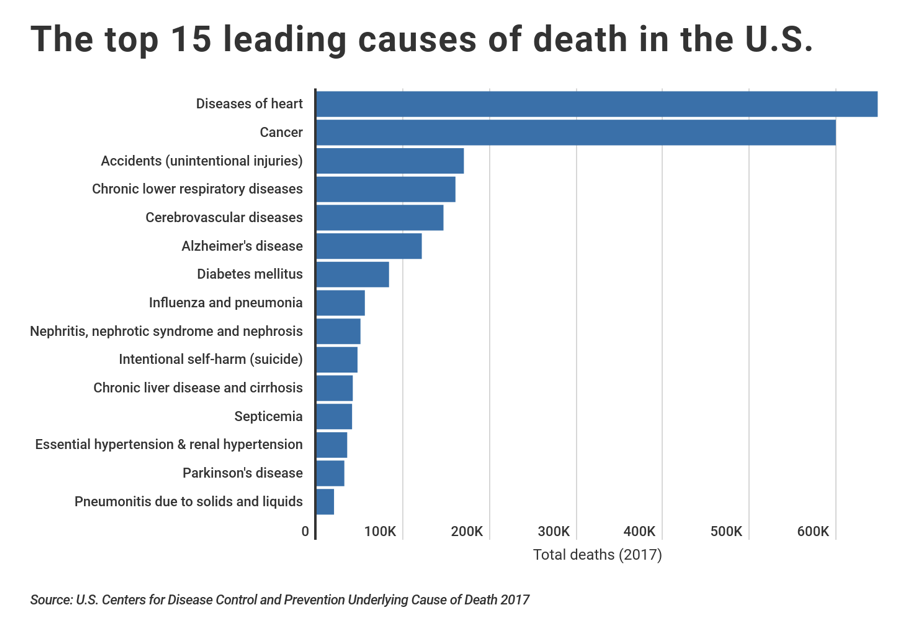
Flu (influenza) deaths this season
- 40,000 USA (range 20,000 to 60,000) (www.cdc.gov/flu/about/burden/pre liminary-in-season-estimates.htm)
- 5,000 CA, estimated. From a population of 40M, if 25% infected with flu virus, this means an infection fatality rate (IFR) of 0.05%. If 12.5% infected, then IFR = 0.1%.
~60,000 flu + pneumonia deaths per year
1.2M heart disease and cancer deaths per year ➔
All-cause deaths: 2.8M per year
Some definitions
COVID-19 stands for “coronavirus disease 2019”
- It refers to the disease, not the virus. In practice, “COVID-19 cases” is used to refer to having a positive 2019 coronavirus lab test regardless of symptoms
- WHO introduced the disease name COVID-19 with great fanfare (after weeks of discussions) at a time when there was no virus name, so it got picked up by the press as the virus name, incorrectly.
- An example of a mis-use is “COVID-19 can survive on surfaces” (https://abcnews.go.com/Health/covid19-days-surfaces-experiment– findings/story?id=69569397), which is nonsensical, technically speaking.
- In addition, COVID-19 is a terrible name for a disease, because you can’t append the word “virus” to describe the pathogen, as ”COVID-19 virus” would mean “coronavirus disease 2019 virus”, which sounds silly and indeed reveals the disease name to lack any informational value whatsoever.
- Previously we named diseases by some sort of description of signs/symptoms, e.g. severe acute respiratory syndrome = SARS. WHO could have named the disease simply “SARS2” and it would have been both accurate and descriptive.
2019-nCOV was the initial name given by some infectious disease organization for the virus, where nCOV stands for novel coronavirus. But this name is hard to remember because it starts with a generic term (the year). It is also inconsistent with coronavirus naming conventions. It is also misleading, because it gives the misimpression that the virus is especially novel. It’s not. In fact it’s the least novel of the respiratory disease- causing viruses isolated in the molecular age. It’s defining feature is it’s NON-novelty…
SARS-CoV-2 is the Genbank name for the virus, because it is 96% identical in nucleotide sequence to SARS-CoV, the cause of SARS in 2003.
- We will use this name because it is accurate and informative, revealing the high similarity between these two pathogens. This name thus reminds us that we can infer a lot about SARS-CoV-2 from existing data on SARS-CoV.
- Ironically, the WHO decided not to name the virus SARS-CoV-2 for precisely this reason – to obscure the relationship between the two viruses (www.vox.com/2020/2/14/21135208/coronavirus-wuhan-china-covid-19-name– sars-cov-2). However we are scientists, we want clarity not obfuscation.
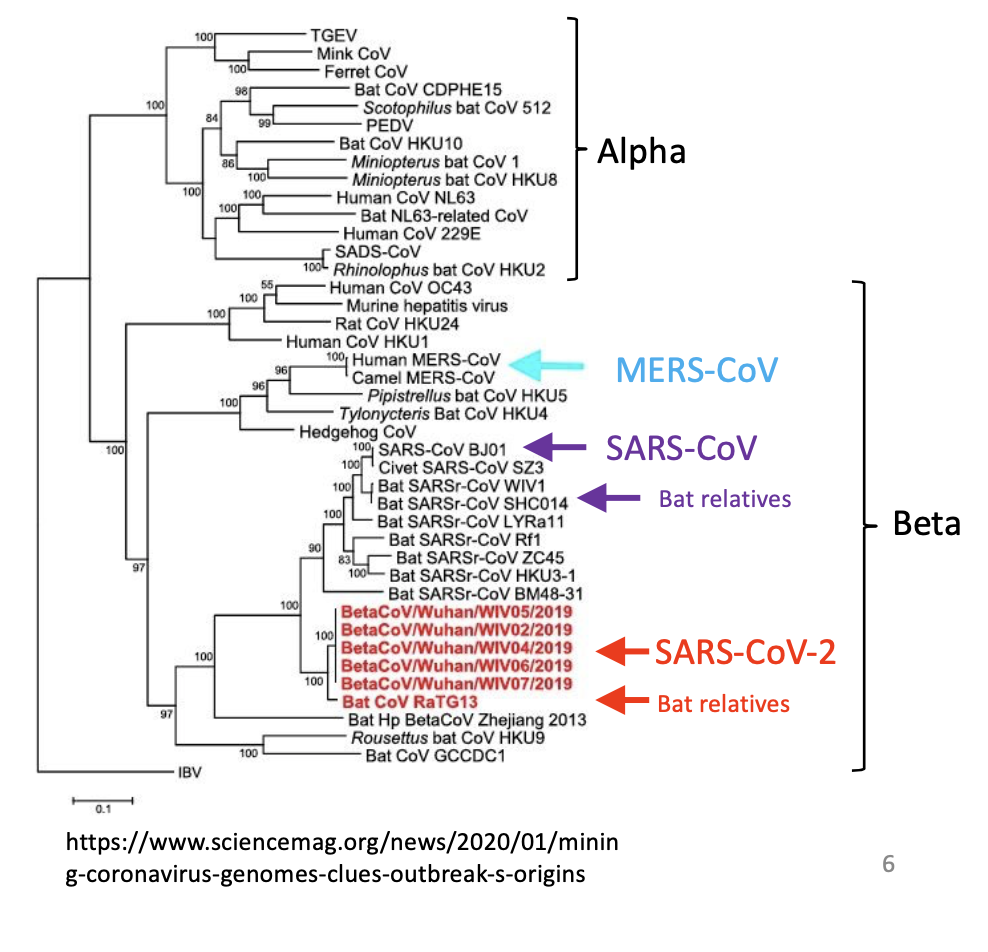
Coronaviruses (CoVs)
- Positive-strand RNA viruses with large genomes (≥27,000 bases).
- Alpha and beta types cause disease in humans.
- Both types already known to cause the common cold, account for 10- 30% of cases (Pubmed 31971553).
- Very stable – CoV OC43 isolates from 1960s and 2001 had only 2 amino acid differences (Pubmed 15280490)!
- Many CoVs in bats.
- Easily hops between species
- MERS-CoV hopped from camels to humans
- SARS-CoV hopped from bats to humans and civets
- SARS-CoV-2 hopped from bats to humans
- It looks like humans with colds gave mice hepatitis, or vice versa).
How might you kill SARS-CoV-2?
- It’s an enveloped virus (with a thin plasma membrane), so easily broken chemically
- Killed by soap/detergents, 60-80% ethanol or isopropanol, Windex (which has detergents), bleach.
- Will be killed by UV, estimated survival in direct sunlight is 10% after 2–3h exposure
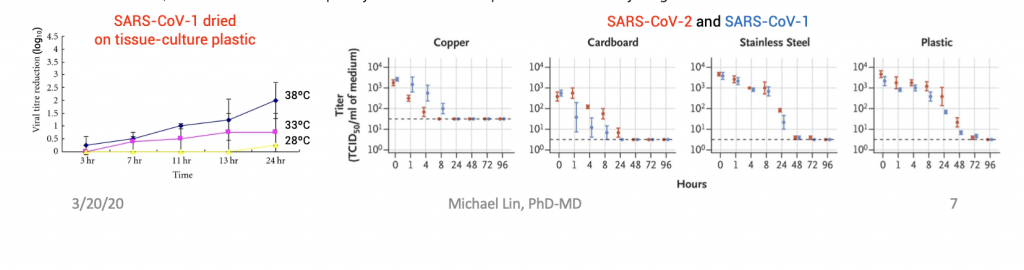
- SARS-CoV-1 is sensitive to temperature, SARS-CoV-2 should be similar
- Survival of SARS-CoV-2 depends on the surface (right, doi.org/10.1056/NEJMc2004973)
- Drop of virus applied, allowed to dry. 1mL cell-culture media applied and tested (equivalent of licking the surface).
- On steel and plastic, 10-fold drop in ~12h. On cardboard (porosity/type unclear, source = “local supplier”), 4–8h.
- On a napkin, the survival should be like on cardboard or lower. Virus should be better trapped by the fluffier napkin fibers, but I still would not wipe my mouth with a napkin that someone just gave me.
How might SARS-CoV-2 kill you?
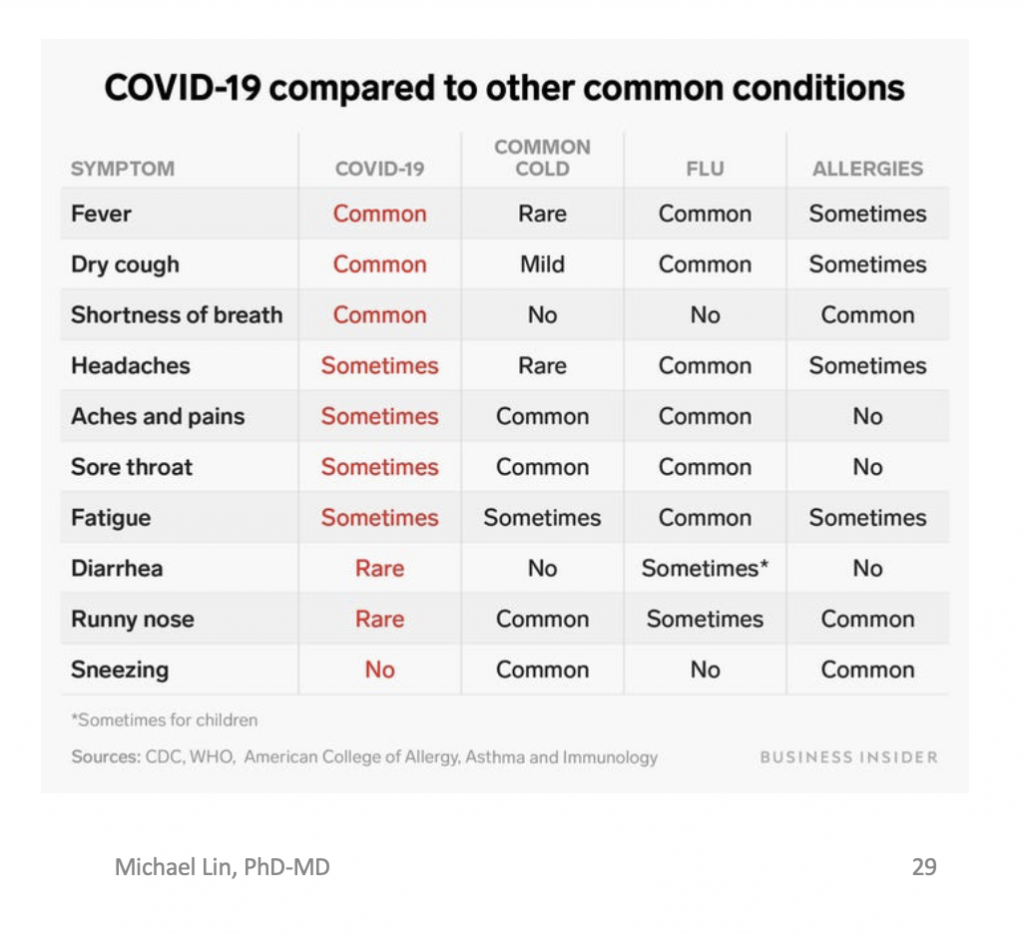
- Initial flu-like symptoms of soar throat, cough, fever, aches, shortness of breath are common. Many people only have these.
- Symptom onset 4-8 days (mean 6 days) after infection
- (www.medrxiv.org/content/10.1101/2020.03.15.20036707v2).
- In severe cases it spreads to lungs causing pneumonia (top)
- Wide variety in symptom severity
- 50% asymptomatic
- 5% severe requiring hospitalization and supplemental O2
- 2.5% requiring ICU and mechanical ventilation 2.5%
- Death 1% due either to alveolar breakdown (ARDS, bottom) ± cytokine release syndrome and multiorgan failure
- Good summaries
- https://www.usatoday.com/in- depth/news/2020/03/13/what-coronavirus-does-body-covid-
- 19-infection-process-symptoms/5009057002/, https://www.nytimes.com/article/coronavirus-body- symptoms.html
Estimating infection (not disease) numbers
- SARS-COV-2 infection numbers matters more than COVID-19 case determines transmission and immunity rate: The higher it is, the more transmission risk but also the more immunity.
- South Korea (SK) has done the most testing per capita.
- In SK, known diagnoses = 8162 on 3/14, new diagnoses ~100 daily now (en.wikipedia.org/wiki/2020_coronavirus_pandemic_in_South_Korea).
- Deaths on average will lag diagnosis by 2 weeks (infections by 3 weeks, wwwnc.cdc.gov/eid/article/26/6/20–0320_article). This is consistent with the shapes of case and death curves, which are updated daily here: (www.worldometers.info/coronavirus/country/south-korea/).
- Thus current total deaths (~75 total on 3/14) occurred from cases diagnosed on 2/29 or earlier, when cumulative number ~ 4000. This means case fatality rate (CFR) ~75/4000 = 1.9%
- However infections > diagnosed cases, so IFR < 1.9%, depending on what fraction of infections were diagnosed on 2/29,
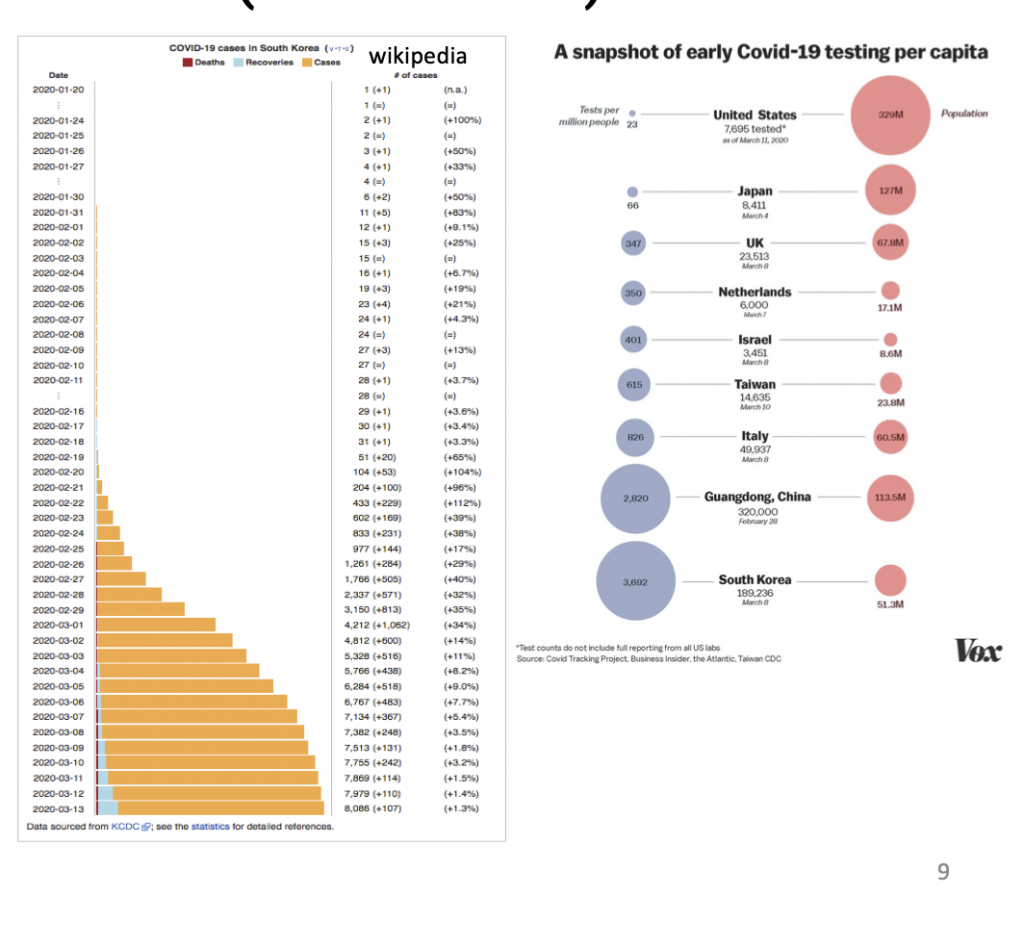
- An analysis of China and the Diamond Princess (DP) gave an IFR of 0.5% for all-China and 1.2% for DP (cmmid.github.io/topics/covid19/severity/diamond_cruise_cfr_estimates.html).
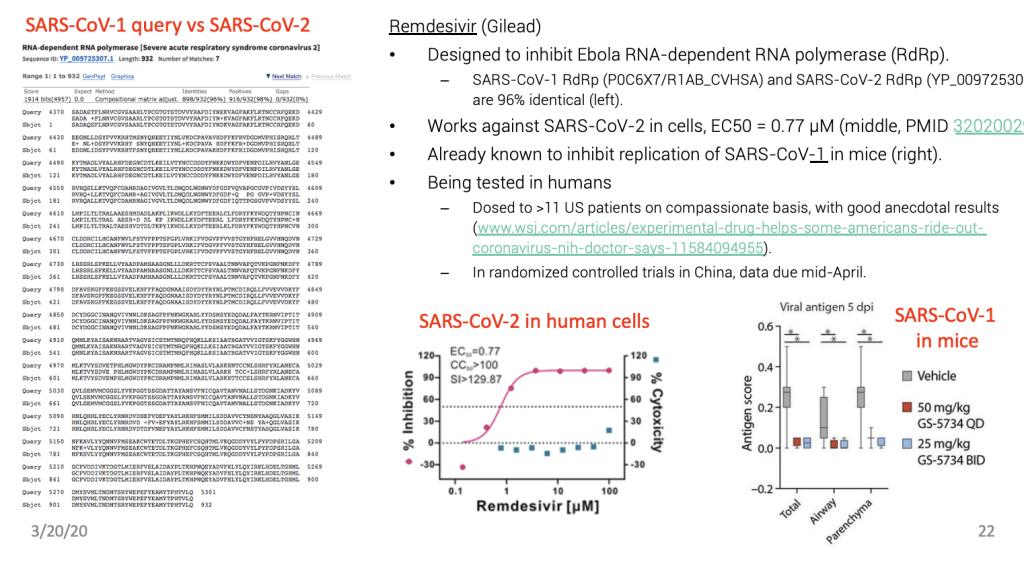
- Note on the DP, some patients may have been helped with the antiviral medication remdesivir (www.wsj.com/articles/experimental-drug-helps-some-americans-ride-out-coronavirus-nih-doctor– says-11584094955) but then DP passengers skewed old.
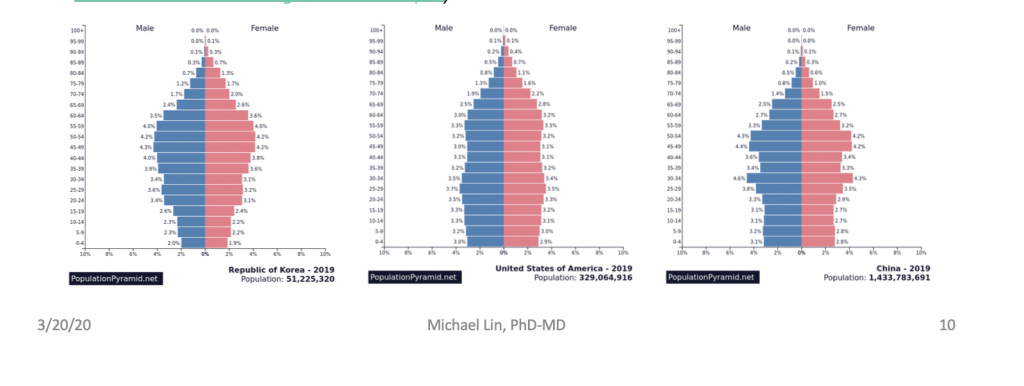
- How would US IFR compare to 0.5% for China and <1.9 for Korea? USA is in between Korea (more) and China (less) in % of population over 60, so we can guesstimate IFR = 1.0%. An estimate based on age-adjusted data from China arrived at a similar IFR = 0.9% (possible range 0.4–1.4) (www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College– COVID19-NPI-modelling-16-03-2020.pdf).
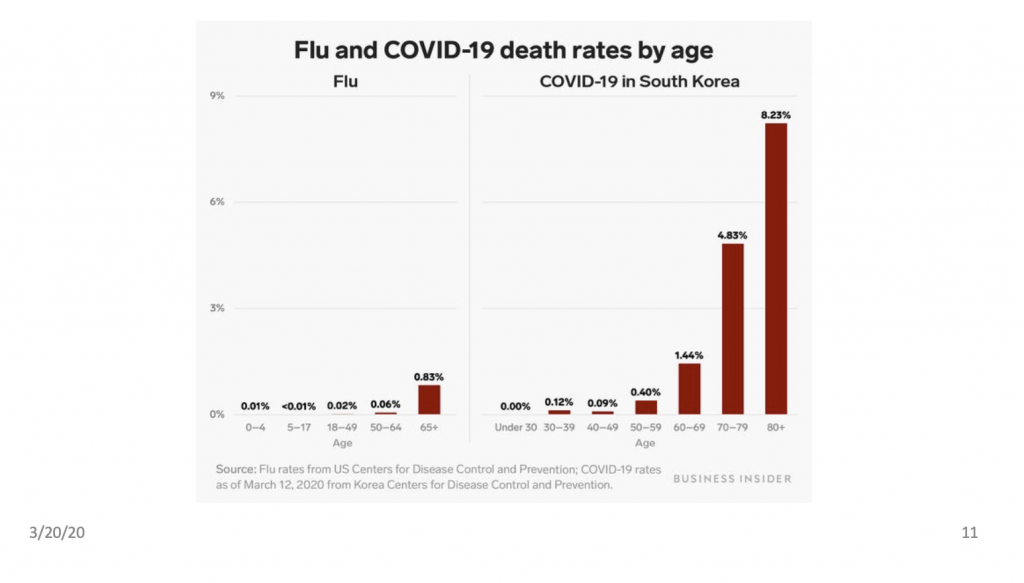
Deaths are mostly in older patients
This is true for both flu and COVID-19
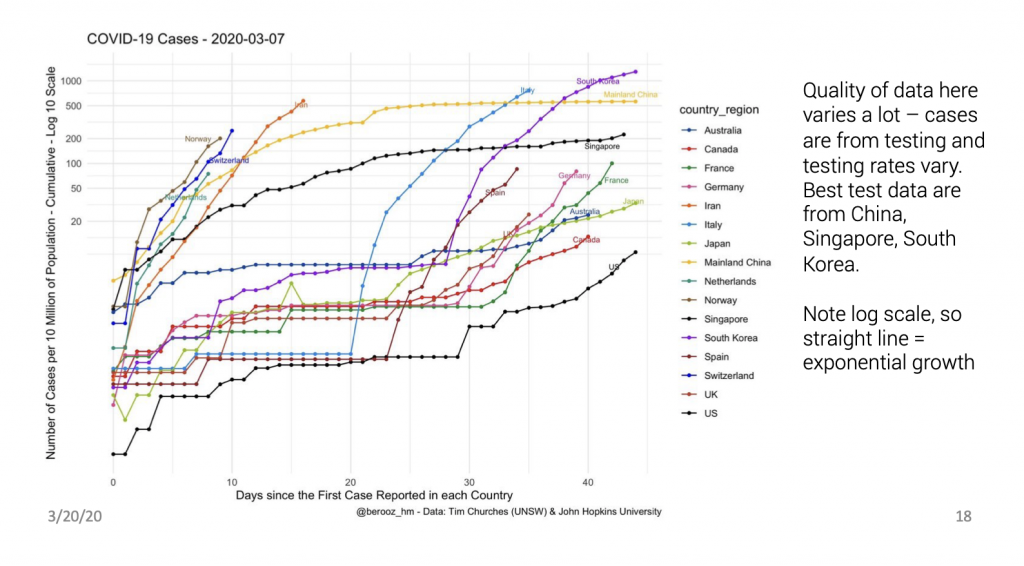
We are still early in the process
Estimating new case rates in CA and Bay Area (updated 2020/3/18)
- 598 confirmed cases and 15 deaths cumulative: 10 this week (Sat-Thurs), 4 last week, 1 two weeks ago (weeks defined Sat-Friday) (www.kcra.com/article/coronavirus– covid19-california-sacramento-latest-information/31406140#).
- 5678 cases in US, so CA is ~1/9th of US, proportional to population.
- Deaths will lag infections by 3-4 weeks (18 days from symptoms but that occurs 3-10 days after infection per www.medrxiv.org/content/10.1101/2020.03.09.20033357v1).
- Assuming constant IFR = 1% with 4-week delay, there were ~1000 infected people in the week ending 4 weeks ago in CA.
- Assuming doubling in new infections each week (average of countries outside China, wwwnc.cdc.gov/eid/article/26/5/20-0146_article), there were 16000 new infections in the last week in CA, which is 1 in 2500 people.
- Let’s assume 8000 (1/2) are in Bay Area. Popn 8,000,000 (1/5 of state) means 1 in 1000 got infected this week in the Bay Area.
What should we do when 1 in 1000 in the Bay Area just got the virus?
- About 50% of patients will be asymptomatic, based on experience with the Diamond Princess (cmmid.github.io/topics/covid19/severity/diamond_cruise_cfr_estimates.html), an estimate from Wuhan data (www.medrxiv.org/content/10.1101/2020.03.03.20030593v1), and an estimate from passengers on evacuation flights (www.medrxiv.org/content/10.1101/2020.03.09.20033357v1).
- Average incubation period is ~7 days. Transmission may begin 2 days before symptoms, so on average at 5 days after infection (www.medrxiv.org/content/10.1101/2020.03.15.20036707v2).
- Thus the 1 in 1000 who just got the virus this week will start spreading virus and then develop symptoms over the next week (obviously not synchronized but continuously over time).
- We can protect ourselves against any undetected spreaders by keeping our hands and common surfaces clean, and maintaining distance when we talk (and use of face masks if you’d like).
- Risk is 1/1000 from direct personal contact; higher from touching fomites in proportion to the number of people touching them between cleanings.
- Take action to reduce a currently low risk of acquiring/transmitting the virus to as low as possible.
How bad could this be?
- If we did nothing and doubling rate remains 1 week, then in worst case, deaths and infections will grow exponentially until virus runs out of people to infect (using CA-only numbers now):
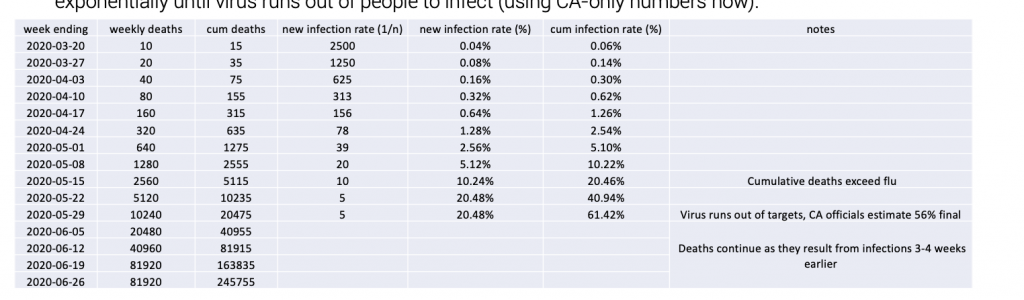
- For US numbers, multiply by 8: ~2M (million) cumulative deaths.
- This is not meant to be numerically accurate, it’s just for illustration, but it fits well the worst-case scenario by an authority in disease modeling (www.nytimes.com/2020/03/20/opinion/coronavirus-outcomes.html).
- You can follow cases (not infection) and fatality numbers at www.worldometers.info/coronavirus/country/us.
- Compare to Spanish flu of 1917-1918: Cumulative infection rate 27%, IFR 2%. Spanish flu might have higher IFR than COVID-19, but medical care was much worse then (no ventilators, no drugs). In reality COVID-19 is likely the more severe disease. In any case, Spanish flu was devastating.
We need to ‘flatten the curve’ now
- Estimated 5% of total infected (not diagnosed cases) require hospitalization and 2.5% require ICU. Average hospital stay is 3 weeks, and starts 2 weeks after infection (1 week after diagnosis) (www.vox.com/2020/3/12/21176783/coronavirus-covid-19-deaths-china-treatment-cytokine-storm-syndrome, www.nytimes.com/2020/03/13/us/coronavirus-deaths-estimate.html).
- Wuhan numbers are 15%/5% of cases, but that is with smoking (60% of males) and pollution (everyone), also infection rate underdetected by 50% (www.medrxiv.org/content/10.1101/2020.03.03.20030593v1).
- Biggest infection surge occurs in the weeks of 5/15, 5/22, and 5/29, when 10%, 20%, and 20% of population = 32M, 64M, and 64M get infected. This will result in 1.6M, 3.2M, and 3.2M needing hospitalization starting 6/7, 6/13, and 6/20. As patients need to stay ~3 weeks, 8M will overlap on the week starting 6/20.
- So we must slow down doubling time from 1 week to ~8 weeks, so hospitalizations peak at <1M.
- So we must slow down doubling time from 1 week to ~8 weeks, so hospitalizations peak at <1M.
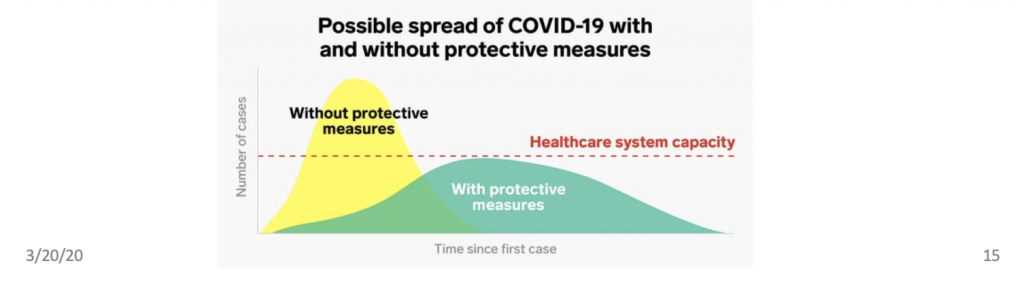
The next month is critical: March 16 to April 16. We must do whatever we can to reduce R0 or increase doubling time. It will take several weeks to know if it’s working.
If we are still doubling each week on April 16, we have only another month to get a second chance.
If that doesn’t work by May 16, there will be no third chance. We would have to immediately clamp down to avoid hospital overflow. This would require Wuhan-like measures such as central quarantine for sick and enforced home-isolation for everyone else.
What can flatten the curve?
- Weather: Maybe 10 ºF increases the doubling time 2x (steady-state reduction in exterior virus levels by 50% per Pubmed 22312351, plus reducing time ×concentration of people indoors).
- Goal is to reduce the reproductive number R0 (how many people infected by each patient).
- Current R0 rate ~ 2 (one person infects 2 others. If they do this in 7 days, it explains doubling time of 1 week).
- Drop R0 to 1.5: Doubling time would increase ~2-fold.
- Drop R0 to 1.25: Doubling time would increase ~4-fold.
- Drop R0 to 1.125: Doubling time would increase ~8-fold.
- Drop R0 to 1.0: Doubling time would become infinite (constant rate of new cases).
- Social distancing, wide testing and tracing, and strict hygiene (face masks, hand sanitizer): This is the approach in SK, Taiwan, Singapore, HK. This seems to have dropped R0 to 1.0 (constant rate of new cases).
- Complete household isolation, immediate quarantining of symptomatic, strict hygiene: This was the approach in Wuhan. R0 dropped from 3.9 to 0.32.
- Is presymptomatic or asymptomatic transmission a factor? Yes, but how much is unclear.
- In Wuhan, R0 fell from 1.3 when symptomatic patients stayed at home to 0.32 when they were centrally quarantined. This suggests only 24% (0.32/1.3) of transmission events occurred before symptoms (www.medrxiv.org/content/10.1101/2020.03.03.20030593v1). But another study estimates 44% of transmission is in presymptomatic period (www.medrxiv.org/content/10.1101/2020.03.15.20036707v2).
- How about asymptomatics? Undiagnosed carriers estimated to be ~55% as infectious as diagnosed cases (doi.org/10.1126/science.abb3221). As undiagnosed carriers are more likely asymptomatic than diagnosed cases, this suggests asymptomatics are not as infectious as symptomatics.
It’s not easy, but social distancing, fast testing, and immediate quarantining can be enough!
Thanks to early research, we already have drugs with activity against the virus
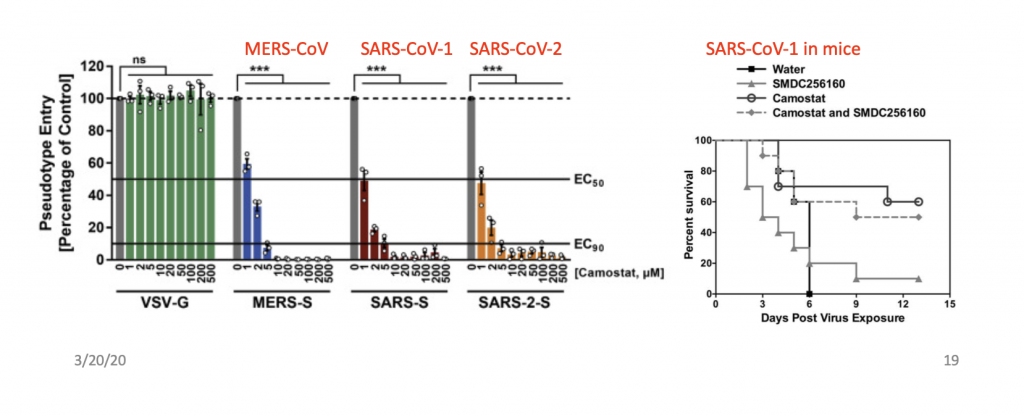
Camostat
- Coronavirus known to require activity of the cellular protease TMPRSS2 for entry, camostat blocks it.
- Inhibits SARS-CoV-2 cell entry with EC50 = 1000 nM (left, from doi.org/10.1016/j.cell.2020.02.052).
- Also helps prevent death in mice with SARS-CoV-1 (right, Pubmed 25666761).
- Camostat approved in Japan for pancreatitis, off-label use possible already.
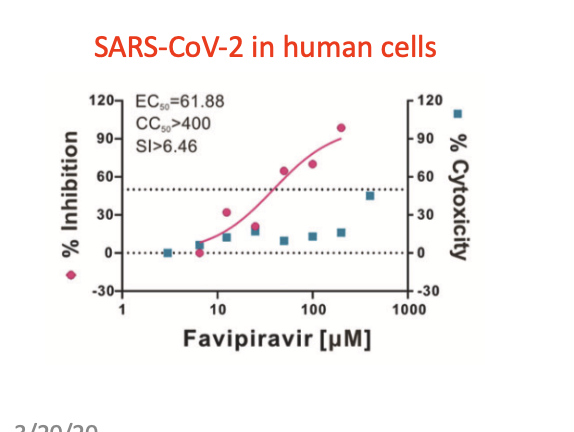
Favipiravir/favilavir/Avigan/T-705 (Fujifilm Toyama)
- Purine analog, gets conjugated to ribose to make a ribonucleoside analog, broad activity against RNA viruses
- Works against SARS-CoV-2 in human cells, EC50 = 61.88 μM (below, Pubmed 32020029). This sounds like relatively poor potency, but Cmax = 400 μM in humans with just oral dosing! (Pubmed 26798032).
- Works in people!
- On 3/17, Chinese authorities announced that favipiravir is effective against COVID-19 in controlled trials, with 8% favipiravir patients vs 17% control requiring ventilators, and 91% vs 62% improving on lung imaging (asia.nikkei.com/Spotlight/Coronavirus/China-says-Japan-developed-drug-Avigan-works-against-coronavirus, www.chinadaily.com.cn/a/202003/17/WS5e708666a31012821727fcbd.html).
- Already approved and stockpiled for influenza outbreaks in Japan (huh, maybe we need to learn from Japan).
Kaletra (lopinavir+ritonavir)
- HIV protease inhibitor approved in multiple countries
- Proposed to target SARS-CoV-2 M protease, required for viral protein processing, but this is not related to HIV protease (www.biorxiv.org/content/10.1101/2020.01.29.924100v1)
- Was used based on anecdotal experience in China, but shown not to work in controlled trial (www.nytimes.com/2020/03/18/health/coronavirus-antiviral– drugs-fail.html)
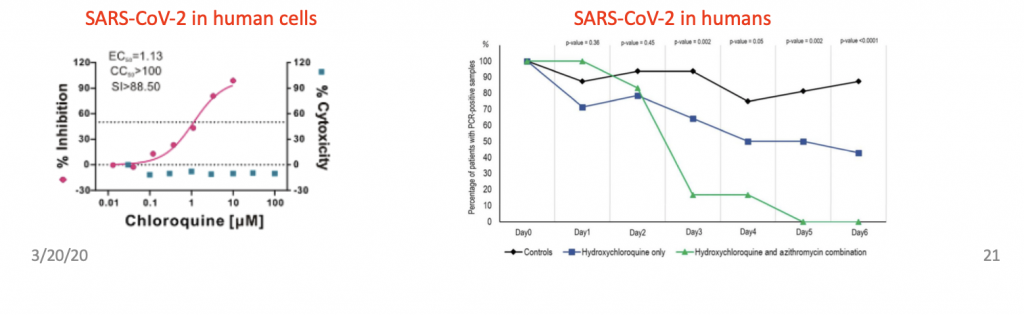
Chloroquine
- Works against SARS-CoV-2 in human cells, EC50 = 1130 μM (below-left, Pubmed 32020029).
- Works against distantly related cold virus CoV OC43 in mice (Pubmed 19506054).
- Works in people!
- 2020-2-17: Per Chinese health ministry news briefing: “results from more than 100 patients have demonstrated that chloroquine phosphate is superior to the control treatment in inhibiting the exacerbation of pneumonia, improving lung imaging findings, promoting a virus- negative conversion, and shortening the disease course” but no data shown (Pubmed 32074550).
- 2020-03-17: Reported effective in reducing viral titers in patients in open-label trial in France: (bottom-right, www.mediterranee- infection.com/hydroxychloroquine-and-azithromycin-as-a-treatment-of-covid-19).
- In trials for preventing infection in China and US (www.startribune.com/university-of-minnesota-to-test-three-drugs-for-covid– patients/568766632/).
- Side-effects can be serious, but it has been safely used for malaria prevention: www.drugs.com/mtm/chloroquine.html.
Remdesivir (Gilead)
Drugs for reducing disease lethality
- Death is often from cytokine release syndrome (cytokine storm) treatment: once virus replicates to high levels in the lungs, the large release of cytokines causes multi-organ failure (www.vox.com/2020/3/12/21176783/coronavirus-covid-19– deaths-china-treatment-cytokine-storm-syndrome).
- Anti-IL-6 mAb Actemra (Roche) was approved for CRS in COVID-19 by China (www.pharmaceutical-technology.com/news/roche– actemra-coronavirus-complications).
- COX-2 inhibitors had been suggested for preventing CRS in SARS but this hasn’t been brought up recently.
- Treating CRS is of course good, but not as good as preventing patients from getting to this point to begin with.
- AT1R blocker losartan is being tested based on a proposal that it will upregulate the SARS-CoV-2 receptor ACE2, preventing loss of ACE2 function which may be protective against the acute respiratory distress syndrome that is one cause of death by COVID-19 (Pubmed 32129518) (www.startribune.com/university-of-minnesota-to-test-three-drugs-for-covid-patients/568766632/).
- This comes from an old hypothesis (2005) that SARS lethality was due to downregulation of ACE2 (www.nature.com/articles/nrd1830) whose validity I’m not too confident about, since it was based on injecting massive amounts of viruses into mice (who can differ from humans in their cardiovascular regulation).
- Others have suggested that upregulating the receptor for the virus with losartan might increase susceptibility to the initial infection (www.thelancet.com/journals/lanres/article/PIIS2213-2600(20)30116-8/fulltext). This probably doesn’t matter either because a virus particle won’t to care if the cell surface it’s swimming on has 100 or 300 receptor molecules to bind to.
- This only deals with lung injury secondary to viral replication, not the virus itself. I think it’s better to concentrate on specific antiviral medications and not worry about the complex ACE2/AT1R pathway.
- More clinical trials here: www.statnews.com/2020/03/19/an-updated-guide-to-the-coronavirus-drugs-and– vaccines-in-development
New treatments and vaccines
- Specific anti-viral antibodies (Vir Biotechnology): made by cloning Ig genes from recovered patients.
- I expect there are already patents filed on synthetic antibody-like molecules isolated against the SARS-CoV-2 envelope proteins by phage display (Regeneron?).
- I also expect there are already remdesivir analogues designed for higher potency on the SARS-CoV-2 polymerase by virtual docking. This is because the SARS-CoV-1 polymerase structure was recently solved by cryo-EM (www.nature.com/articles/s41467-019-10280-3), so the SARS-CoV-2 structure can then be easily predicted (www.biorxiv.org/content/10.1101/2020.01.29.924100v1)
- There are likely many other drugs being designed based on virtual screens, e.g. www.drugdiscoveryonline.com/doc/stonewise-ai-driven-drug-discovery-polymerase-inhibitors-covid-infection– treatment-0001
- Many vaccines in development, fastest are RNA-based (CureVac, Moderna) www.chemistryworld.com/news/rna– vaccines-are-coronavirus-frontrunners/4011326.article
- Some more summary and speculation here: doi.org/10.1021/acscentsci.0c00272
- Why not vaccinate with formalin inactivated virus like the first polio vaccine?
- An inactivated SARS-CoV-1 vaccine was protective in monkeys (Pubmed 15837221).
- This has been proposed for SARS-CoV-2 (www.nature.com/articles/s41541-020-0170-0); I hope someone is trying it. If CDC is doing their job, they should already be making such vaccines in-house AND TELLING US ABOUT IT. Which gets me to the next point…
How CDC and FDA Failed
- CDC was initially inflexible on testing guidelines (e.g. needed travel or exposure history).
- CDC created a test requiring a slow RT-PCR reaction on a specific model of machine, designed poor primers, and didn’t realize this for a month. This was both strategically (using 30-year-old technology) and tactically (designing bad primers) incompetent. I would expect most graduate students to do better.
- FDA was inflexible on tests: approved only the (initially flawed) CDC test, refused working tests from WHO and other countries (www.cnn.com/2020/03/12/asia/coronavirus– south-korea-testing-intl-hnk/index.html), even required CDC to retest results of other labs (www.propublica.org/article/the-fda-is-forcing-the-cdc-to-waste-time-double– testing-some-coronavirus-cases)
- Finally allowed academic labs to develop their own tests on 2/29 (www.aamc.org/news- insights/coronavirus-testing-how-academic-medical-labs-are-stepping-fill-void)
- Finally approved rapid Roche test on 3/13 (www.fiercebiotech.com/medtech/fda-grants– roche-coronavirus-test-emergency-green-light-within-24-hours)
- CDC being too slow to understand and discuss treatments and vaccines
- Already approved drugs like chloroquine, favipiravir, and Kaletra can be used off-label without FDA re-approval, and doctors look to CDC for guidance.
- CDC could have persuaded or contracted with drug manufacturers to produce more of these upon first indication of their efficacy, to be prepared.
- It seems CDC did no such thing, as US manufacturers are only starting up chloroquine production now, after its mention in a White House press conference on 3/19 (newsroom.mylan.com/2020-03-19-Mylan-Ramps-Up-U-S-Manufacturing-of- Hydroxychloroquine-Sulfate-Ta blets-to-Meet-Potential-COVID-19-Patient-Needs).
- This contrasts with Chinese companies who restarted production 1 month ago, 1 day after trial results (yicaiglobal.com/news/guangzhou-pharma-taps-old-antimalarial– drug-after-covid-19-use-is-proven).
- Providing non-information in place of information. Example from CDC website (www.cdc.gov/coronavirus/2019-ncov/specific-groups/children-faq.html)
- Q: What is the risk of my child becoming sick with COVID-19?
- A: “Based on available evidence, children do not appear to be at higher risk for COVID-19 than adults. While some children and infants have been sick with COVID-19, adults make up most of the known cases to date. You can learn more about who is most at risk for health problems if they have COVID-19 infection on CDC’s current Risk Assessment page.”
- Better answer: “Children have milder disease courses than adults, although they may still transmit the disease at low efficiency to adults.” It’s clear that kids get less sick if at all. Why doesn’t the CDC say so? It won’t hurt to tell the truth! If you provide such lousy information, people will stop trusting you.
How White House failed
- Not learning the facts well enough to make useful decisions such as ordering FDA to approve other tests and CDC to expand testing guidelines.
- Not learning the facts well enough to become trustworthy to the public.
- Not explaining to the public why social distancing is necessary to protect the elderly.
- Not explaining to the public that social distancing does NOT mean disruption to food and supplies as long as people don’t hoard.
- Not motivating people to do their part by (1) stepping up hygienic habits, (2) limiting non-essential activities that can spread the disease, and (3) not hoarding resources. Instead the press and local officials have taken the initiative to do this, but this creates the problem of too many information sources.
- Hogging the spotlight instead of naming a trusted doctor or scientist to be the face of policy. Should have made sure Fauci was given the most attention by the press.
Overall a complete lack of analysis/judgment/foresight by leadership at FDA/CDC/WH
Recommendations – health
- At the first sign of CoVID19 symptoms (right), stay away from others and get tested. Put on a mask and keep your hands clean in the presence of others until you know your test results.
- Recall the worry is about transmitting virus to older people, even if you have mild symptoms you do not want to transmit the virus to others.
Recommendations – hygiene
- Don’t shake hands and stay 6 ft away from people outside your household – these are easy.
- But ”wash your hands often” and “don’t touch your face” are confusing without context – how often is often? Why can’t I touch my face? Should I ask someone to scratch my itchy nose for me? Shouldn’t I also worry about what I’m touching, not just my hands? If so, what cleaning solutions should I use?
- I’ll provide some details. I treat hands and objects similarly, and I am pretty strict:
- To protect yourself, sanitize your hands right before eating and right after touching things touched by others.
- To protect others, use clean hands to touch others’ things or when handling things to others.
- Sanitize objects you get, and only give out sanitized objects. For example, I have hand sanitizer open and ready to clean my credit card right after I get them back from cashiers, before I put it back in my wallet.
- Outside your house, sanitize smooth surfaces you will touch directly with your hands (e.g. tables and chair edges, wherever you put your phone and computer).
- I keep track of whether hands/objects are clean. As long as they have not encounted unknown/dirty things after their last cleaning, they don’t need to be recleaned. This is why I suggest immediate sanitation of hands after touching unknown/dirty things, so you can resume using your clean things without worry.
- You can open doors with your body or foot, and use paper towels to handle faucets or knobs.
- Create clean zones – your house, your office (if you’re allowed to work), your car.
- Sanitization can be done by soap and water (hands) or hand sanitizer (hands or objects) or Windex (objects).
- “Disinfectants” like bleach or quarternary amines are for large areas for which soap (due to the need to rinse) or alcohol (due to fumes, expense) are not practical. If you can use soap or alcohol, you don’t need them.
- Finally, if your hands are clean, you can touch your face! But remember to sanitize them before you touch other people’s stuff.
Recommendations – face masks
Face masks: yes or no?
- You will see news articles saying that you don’t need face masks as they are largely ineffective, or that you shouldn’t buy face masks because caregivers need them.
- These statements cannot both be true! If face masks are ineffective why do caregivers need them?
- Well, they are effective (www.nytimes.com/2018/03/23/well/live/face-masks-work-healthy-colds– flu-immunity-prevention.html)
- In addition to spreading through contact and then ingestion, SARS-CoV-2 also spreads through inhalation of airborne droplets.
- Disposable masks are filters, causing bacteria and droplets to be caught in a meshwork of polypropylene. They are not rated for completely filtering out aerosolized viruses, i.e. individual viruses in a small water shell. There is some evidence SARS-CoV-2 can be aerosolized, but its mode of spread is mostly through larger droplets.
- Masks absorb 95% of exhaled droplets from infected people (Pubmed 2 3505369).
- Masks also absorb droplets during inhalation; this is harder to quantify but certainly substantial, as masks cut transmission within households by 60-80%, a situation with lots of viral droplets around (Pubmed 19193267) .
- Both surgical masks and N95 respirators are effective (Pubmed 19797474), although it’s assumed the N95 are better.
- My recommendations for mask usage are based on relative risks
- At current infection rates and in normal activities, most people would be wasting masks.
- But masks would be useful in proximity with strangers (airplane, train, Uber/Lyft, and especially hospital or clinic).
- They are warranted for at-risk people, i.e. the immunocompromised or elderly, in public.
- If the infection rates climb then they would be useful for everybody out in public.
- They are absolutely recommended for people who are sick for avoid transmitting viruses.
- Mask use is controversial because of limited supply
- To assure those who need masks most get them, try to conserve them, and buy a small supply.
- It is better to do social distancing without masks than social crowding with masks. In Asia, where most people take public transport, masks are considered a necessity and are handed out by authorities.
- Given that some people are more at-risk, there should be no stigma/shaming for wearing masks.
- 3/19 update: my views have now been validated by a former FDA commissioner: https://twitter.com/ScottGottliebMD/status/1240243298725486592. You can only deny facts for so long.
- What if you don’t have masks, and the stranger next to you is coughing?
- You can breathe through the sleeve of your shirt in your elbow.
- You’d do this anyway in a smelly or smoky location, right? That means it’s effective at blocking small particles.
- Indeed, a T-shirt blocks 70% of virus-sized particles, which is better than nothing (www.researchgate.net/publication/258525804_Testing_the_Efficacy_of_Homemade_Masks_Would_They_Protect_ in_an_Influenza_Pandemic)
- How to use masks
- Make sure to clean your hands well before putting on or taking off masks.
- For the soft surgical masks, bend the hard edge to fit your nose (colored side out), put on your nose and pull the straps over your ears, then stretch the mask down to cover your chin.
- How to conserve face masks
- Disposable masks are meant to be worn “once” then throw away, but once is not defined. To conserve, it’s reasonable to use one mask one day if you’re not seeing patients. (Quarantine officials forced Grand Princess passengers to use one mask for 9 days: reut.rs/39RVWuy. I would not recommend that at all.)
- When alone, use clean hands to lower the mask to your chin. This gives a chance for the mask to dry out, which makes it more effective. You can also do the same when you need to drink.
- When eating, you don’t want stuff dropping from the mask onto your food, so remove the mask completely and set in a clean place outside-up.
- As the outside of a used mask is potentially dirty, you should clean your hands after touching it, or you can have your hands wet with hand sanitizer the whole time you handle it.
- To clean and reuse masks, place in oven at 70ºC = 160ºF for 30-60min, or expose both sides in a UV sterilizer. Alcohol is not recommended (mp.weixin.qq.com/s/3QYVWO4kj5qwuSHnhcM9uQ). 3/20 update: Before rule-lovers complain, I’ll point out that UV sterilization and reuse of masks is now being done by hospitals (www.nytimes.com/2020/03/20/health/coronavirus-masks-reuse.html). Funny how single-use rules promoted by manufacturers are taken as inviolable truth, until they are revealed as not.
Recommendations – activities
- It’s okay to go out to buy essentials, get takeout, but assume anything can be carrying virus, so practice good hygiene as above, i.e. maintain 6ft separation, sanitize hands in between touching others’ things and your own things, pass only clean objects, and treat objects you acquire as dirty. Visiting the workplace should be fine if you work mostly alone and can take the same hygiene steps above. (3/19 update: CA citizens cannot go to workplaces except for some essential jobs.)
- It’s okay to see relatives who are not sick to provide help, but again only if you can practice good hygiene. Limit duration and closeness of visits to elderly or immunocompromised relatives.
- I have reversed my allowance for social visits to friends, given that many feel it’s uncool to practice good hygiene such as wearing face masks, not touching common objects. (3/19 update: Also not allowed in CA anymore.)
- Buy groceries online. Ironically stay-in orders increase transmission risk at grocery stores, which are now packed. My estimate is 1 in 1000 might carry infections by early April. That number can pass through one store daily. If you must go, stay 6ft from others and sanitize hands and purchases!
- I suggest avoiding prepared salads or sandwiches, and retoasting/microwaving that pastry.
- Don’t share food, obviously.
- Go outside – sunlight is the best disinfectant.
- Do safer activities – this is not the time you want to break a leg and have to go to the hospital.
Recommendations – travel
- Large meetings that bring people from around the country
arewere obviously a big risk:- Large numbers of people who might breath the same air and touch the same things (e.g. at Biogen meeting, attendants used the same serving utensils at a buffet, and 70 got infected).
- These people tend to travel many times so they can spread viruses further.
- Viruses can be collected from many locations and transmitted to many others (e.g. Biogen).
- Thus non-urgent meetings should be cancelled.
- 3/16 update: Obviously no more conferences/festivals for a while.
- Travel if you must, e.g. to help care for family (3/17 update: removed nonessential travel in compliance with most health officials’ directives). Students also need to go home! But due to the many points when exposure from strangers can occur, travel requires high vigilance. For example, sanitizing items that others give to you now includes your ID at the TSA checkpoint and the can of soda from the flight attendant. Sanitizing surfaces you touch now include tray tables, seat belts, armrests. Keeping your hands clean when touching your own things now means washing hands after closing the airplane bathroom door (because you don’t want germs on your zippers) and, after washing hands after finishing, opening the same door with your elbow (or a napkin). Make sure the ventilation nozzle is on full blast (it puts out HEPA-filtered air) – sanitize it or your hands after touching it, of course.
- Similar hygienic tips apply to trains and buses and cars that are not your own.
- A face mask would be useful in cars with others, trains, planes, crowded waiting areas.
No need to worry about supplies
- 50% of people with virus have no symptoms but will become immune, just like most symptomatic people
- 95% don’t need to go to the hospital
- The workforce is not threatened
- Farmers and truck drivers and store workers will be available for work
- You don’t need to buy everything in sight
- This is not the zombie apocalypse
Hand sanitizer recipe
- Hand sanitizer is just 60-70% ethanol with moisturizers.
- The ethanol you want to use is 95% non-denatured ethanol
- 95% denatured ethanol has toxic additives to prevent drinking (will have a health hazard logo).
- 100%/dehydrated/absolute/anhydrous ethanol has benzene, also toxic, from the purification process.
- Isopropanol can be substituted for ethanol, but just takes longer to evaporate
- 60-70% isopropanol is just as effective as 60-70% ethanol as a disinfectant.
- 99-100% isopropanol (rubbing alcohol) can be purchased by the consumer as a cleaning and disinfecting agent.
- The moisturizer can be aloe vera gel (available in drugstores) or glycerol (a common lab reagent, and an ingredient in moisturizers and makeup).
Lin Lab recipe: Mix two parts 95% non-denatured ethanol or 99-100% isopropanol with 1 part aloe vera gel or 90-100% glycerol. That’s it!
(Thanks to Yichi Su for testing, and Michael Westberg for the safety tips)